There have been some remarkable developments in immune therapy in oncology during the past year. Monoclonal antibody therapy, checkpoint inhibitors and vaccine therapy are rarely out of the scientific and popular media.
It is also possible to target cancer by the transfer of effector cells as a form of ‘passive’ immune therapy. But even a few years ago, this approach may have seemed an unlikely one, in practical terms. But now adoptive immune cell therapy is becoming realised. But what is driving this?
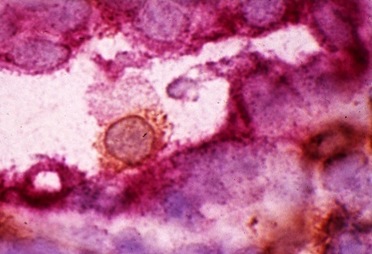
ACT: Adoptive cell transfer (ACT) is a technique that can be applied to the transfer of immune cells, including T-lymphocytes (or T-cells). ACT therapy is much more difficult to implement than monoclonal antibody therapy. ACT involves removing a patient’s T-cells, enhancing the cells’ activity and then re-introducing these ‘activated’ T-cells to enhance a patient’s anti-tumour response.
ACT was initially developed to utilise tumour-infiltrating lymphocytes (TILs) from surgically excised samples of metastatic melanoma. The melanoma-specific T-cells within the TIL preparation were expanded ex vivo via co-culture melanoma cells in the presence of the interleukin-2 (IL-2). The expanded T-cell populations and their products were then administered back to the patient. There have been some remarkable results from ACT, with tumour shrinkage even in very large tumours. The process of sampling and expanding TIL was feasible in melanoma, which is highly immunogenic, but not in other cancers.
One solution to the problem of TIL collection was to collect naive T-cells from peripheral blood and to engineer them to express cancer antigen-specific receptors.
CARs: Chimeric antigen receptors (CARs) are composed of an antigen-binding variable fragment from monoclonal antibodies fused to intracellular T-cell signalling domains from signalling molecules. CARs are synthetically engineered using CRISPR (clustered regularly interspersed short palindromic repeats) technology and lymphocytes or haematopoietic stem cells. CARs target native cell-surface antigens in an MHC-independent manner. This technique allows for the generation of a ‘universal product’ for patients.
CAR-T or CAR/ACT: Chimeric antigen receptor transduced (adoptive) T-cell therapy modifies patients’ immune cells to fight cancer cells. Chimeric antigen receptor (CAR)-expressing T cells have demonstrated clinical efficacy in patients with B-cell leukaemia expressing the differentiation antigen CD19. In a recent phase 1 dose-escalation study in children and young adults with acute, B-cell, lymphoblastic leukaemia (ALL), CD19-CAR T-cell therapy was feasible, safe, and mediated anti-leukaemic activity; any reported toxicity was reversible and prolonged B-cell aplasia was not present.
In January 2015, the profile of CAR-T therapy was raised following the announcement of some high-profile collaborations between pharmaceutical and biotechnology companies and manufacturing companies. These collaborations have the main aim of steering immune therapy in oncology towards applied immune synthetic biology.
Firstly, Novartis, the University of Pennsylvania and Intellia have announced a programme to develop synthetically engineered CAR-Ts. Second, Cardio3 BioSciences have acquired the OnCyte CAR T-cell portfolio from Celdara, who has several CAR T-cell therapeutic products in development. Third, Amgen have partnered with Kite Pharma, who has an established CAR platform with manufacturing facilities.
CAR therapy is an approach that could become applicable to all forms of cancer. Several phase 1 clinical trials are now in progress using the CAR approach. It is likely that this year will see pharmaceutical and biotechnology competitors rallying to see whose CARs can reach the ‘therapeutic finish line’ first.
It is also possible to target cancer by the transfer of effector cells as a form of ‘passive’ immune therapy. But even a few years ago, this approach may have seemed an unlikely one, in practical terms. But now adoptive immune cell therapy is becoming realised. But what is driving this?
ACT: Adoptive cell transfer (ACT) is a technique that can be applied to the transfer of immune cells, including T-lymphocytes (or T-cells). ACT therapy is much more difficult to implement than monoclonal antibody therapy. ACT involves removing a patient’s T-cells, enhancing the cells’ activity and then re-introducing these ‘activated’ T-cells to enhance a patient’s anti-tumour response.
ACT was initially developed to utilise tumour-infiltrating lymphocytes (TILs) from surgically excised samples of metastatic melanoma. The melanoma-specific T-cells within the TIL preparation were expanded ex vivo via co-culture melanoma cells in the presence of the interleukin-2 (IL-2). The expanded T-cell populations and their products were then administered back to the patient. There have been some remarkable results from ACT, with tumour shrinkage even in very large tumours. The process of sampling and expanding TIL was feasible in melanoma, which is highly immunogenic, but not in other cancers.
One solution to the problem of TIL collection was to collect naive T-cells from peripheral blood and to engineer them to express cancer antigen-specific receptors.
CARs: Chimeric antigen receptors (CARs) are composed of an antigen-binding variable fragment from monoclonal antibodies fused to intracellular T-cell signalling domains from signalling molecules. CARs are synthetically engineered using CRISPR (clustered regularly interspersed short palindromic repeats) technology and lymphocytes or haematopoietic stem cells. CARs target native cell-surface antigens in an MHC-independent manner. This technique allows for the generation of a ‘universal product’ for patients.
CAR-T or CAR/ACT: Chimeric antigen receptor transduced (adoptive) T-cell therapy modifies patients’ immune cells to fight cancer cells. Chimeric antigen receptor (CAR)-expressing T cells have demonstrated clinical efficacy in patients with B-cell leukaemia expressing the differentiation antigen CD19. In a recent phase 1 dose-escalation study in children and young adults with acute, B-cell, lymphoblastic leukaemia (ALL), CD19-CAR T-cell therapy was feasible, safe, and mediated anti-leukaemic activity; any reported toxicity was reversible and prolonged B-cell aplasia was not present.
In January 2015, the profile of CAR-T therapy was raised following the announcement of some high-profile collaborations between pharmaceutical and biotechnology companies and manufacturing companies. These collaborations have the main aim of steering immune therapy in oncology towards applied immune synthetic biology.
Firstly, Novartis, the University of Pennsylvania and Intellia have announced a programme to develop synthetically engineered CAR-Ts. Second, Cardio3 BioSciences have acquired the OnCyte CAR T-cell portfolio from Celdara, who has several CAR T-cell therapeutic products in development. Third, Amgen have partnered with Kite Pharma, who has an established CAR platform with manufacturing facilities.
CAR therapy is an approach that could become applicable to all forms of cancer. Several phase 1 clinical trials are now in progress using the CAR approach. It is likely that this year will see pharmaceutical and biotechnology competitors rallying to see whose CARs can reach the ‘therapeutic finish line’ first.
 RSS Feed
RSS Feed