End-of-year reviews serve to highlight what is new or what has been headline news during the past year with some predictions or hopes for the coming year. In the case of hyperlipidaemia therapy, 2014 brought three main clinical developments.
Firstly, a new approach to the removal of ‘bad’ LDL-cholesterol (LDL-C) from the blood includes a novel class of therapeutic monoclonal antibody inhibitors (to the enzyme PCSK9) that show promise in clinical trials.
Second, the safety and efficacy of statin therapy have been re-evaluated, with new recommendations for more widespread use and combination treatment approaches.
Third, 2014 saw the publication of new clinical guidelines on the management of hyperlipidaemia from the National Institute for Health and Care Excellence (NICE), the American College of Cardiology/American Heart Association (ACC/AHA), the European Atherosclerosis Society (EAS), the International Atherosclerosis Society (IAS) and the American Diabetic Association (ADA)..
As for 2015, the race is on for regulatory approval of new potential cardiology ‘blockbuster’ drugs to control hyperlipidaemia. Further into the future comes the possibility of inhibiting the lipid-regulating enzyme, PCSK9, using targeted gene therapy.
THE CASE FOR HYPERLIPIDAEMIA TREATMENT
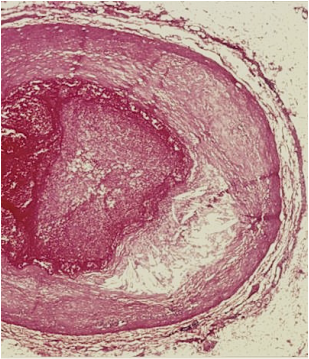
Cardiovascular disease remains the most common cause of morbidity and mortality worldwide. The underlying disease, atherosclerosis, affects large muscular arteries such as the coronary arteries and also the aorta. Coronary artery atherosclerosis, or coronary artery disease (CAD) causes acute and chronic ischaemic heart disease (IHD), including myocardial infarction (MI) or ‘heart attacks.’
Familial hypercholesterolaemia (FH) is caused mainly by genetic defects in the LDL receptor gene. This genetic defect impairs the ability of the liver to remove LDL-C from the blood. The heterozygous form of the defective gene is inherited from one parent and affects between 1 in 250 and 1 in 300 people worldwide, which makes heterozygous FH one of the most common hereditary condition in humans. The homozygous form of FH is more severe and occurs when a mutated copy of the gene is inherited from both parents and affects between 1 in every 500,000 to 1 in every one million people.
Aside from familial forms of hyperlipidaemia, individuals who are also considered to be at risk of coronary artery disease (CAD) and who are advised to control plasma LDL-C levels include those with diabetes mellitus, hypertension, obesity and smokers.
STATIN THERAPY
For the past two decades, statin therapy, including atorvastatin (Lipitor®) and its generic forms, rosuvastatin (Crestor®) and recently ezetimibe (Zetia®), has been the mainstay of treatment to lower this ‘bad’ cholesterol (LDL-C). In November 2014, the outcome of the IMPROVE-IT clinical trial, an 18,144-patient study of high-risk patients presenting with acute coronary syndromes, showed that patients taking ezetimibe (Zetia®) in combination with simvastatin (Vytorin®) experienced significantly fewer major cardiovascular events.
The dominance of statin therapy in hyperlipidaemia has persisted despite the fact that some patients will be resistant and will maintain high LDL-C levels with treatment while some others will be unable to tolerate statins.
2014 was a year when lowering plasma cholesterol with statins was a key topic in the general media as well as in the medical journals. It was also a year of controversy regarding the safety of statin therapy. In the British Medical Journal (BMJ) meta-analysis data was reported to show that only a small minority of adverse symptoms in patients taking statins were genuinely due to the statins. This media attention came at a time when NICE issued its draft guidance recommending lowering the risk threshold for starting statin treatment. A leading UK epidemiologist stepped in to caution against widespread statin prescribing.
While much of the media attention given in 2014 to hyperlipidaemia treatment was directed at statin therapy, there were some new developments.
PCSK9 INHIBITORS
The enzyme proprotein convertase subtilisin/kexin 9 (PCSK9) is a serum protease, the ninth member of the subtilisin family of kexin-like proconvertases to be identified. PCSK9 sequesters the LDL-cholesterol (LDL-C) receptor in the liver and so reduces plasma levels of LDL-C. In early clinical trials, the reduction in plasma LDL-C that follows PCSK9 inhibition has been shown to be greater (by up to 80%) than with statins alone and PCSK9 have been reported to have fewer side effects. This initial efficacy and safety data explains why the PCSK9 inhibitor class of drugs are predicted to be the next blockbusters in cardiology and why there is a race to develop these inhibitors.
A. PCSK9 Monoclonal Antibody Therapy
PCSK9 inhibitory therapeutic monoclonal antibodies include alirocumab (Sanofi/Regeneron), evolocumab / AMG 145 (Amgen) and bococizumab (Pfizer). These humanized monoclonal antibodies bind to PCSK9. The interest in this therapeutic approach lies in the fact that a single injection may be effective when given weekly, fortnightly or even monthly.
Alirocumab: In October 2013, alirocumab showed promising clinical data in phase 3 clinical trials. The ODYSSEY programme included 12 trials that included more than 23,000 patients with either familial hyperlipidaemia or intolerance to statin therapy. The ODYSSEY MONO trial compared alirocumab with ezetimibe at week 24, with results showing mean LDL-C reductions from baseline of 47.2% on treatment with alirocumab when compared with 15.6% with ezetimibe. In phase 2 trials, alirocumab combined with a statin achieved LDL-C reductions in up to 73% of patients.Preliminary data from the ongoing Odyssey Long Term study, showed that alirocumab halved the number of strokes and heart attacks in heterozygous familial hypercholesterolemia and high-risk cardiovascular patients (1.4 % of alirocumab-treated patients compared with 3% for placebo). Regulatory filings for alirocumab in Europe and the USA are expected during 2015.
Evolocumab (AMG 145): Evolocumab is a humanized therapeutic monoclonal antibody that inhibits PCSK9. Safety and efficacy of evolocumab is being evaluated in a programme of 22 phase 3 clinical trials involving more than 30,000 patients. Evolocumab is administered every two weeks and monthly in multiple patient populations. The name of the programme is PROFICIO (Program to Reduce LDL-C and Cardiovascular Outcomes Following Inhibition of PCSK9 In Different Populations).
Data from the ongoing PROFICIO phase 3 trials, the large MENDEL-2 phase 3 trials in statin-naîve patients and in the GAUSS-2 phase 3 trial in statin-intolerant patients, evolocumab reduced LDL-C levels by more than 50%.Data from the RUTHERFORD-2 clinical trial, published in October 2014, showed that evolocumab was well-tolerated in patients with heterozygous familial hypercholesterolaemia, and gave significant reductions in LDL-C compared with placebo.Data was analyzed at 52 weeks from the DESCARTES long-term safety and efficacy clinical trial in patients with hyperlipidemia at risk for cardiovascular disease. Evolocumab treatment when added to the diet alone, to low-dose atorvastatin (Lipitor®), or to high-dose atorvastatin (Lipitor®) with or without ezetimibe (Zetia®) significantly reduced LDL-C levels.
Following the results of these clinical trials, Amgen has become the first company to seek regulatory approval for a PCSK9 inhibitor. In August 2014, a submission was made of a biologics license application (BLA) to the US Food and Drug Administration (FDA). In September, 2014, a submission of a Marketing Authorization Application (MAA) was made to the European Medicines Agency (EMA). The result of these filings is expected during 2015.
Bococizumab (RN-316): For Pfizer’s therapeutic monoclonal antibody, bococizumab, ongoing large phase 2 and phase 3 clinical trials are due for completion during 2015 and 2016. The safety, efficacy and tolerability of bococizumab is being assessed in more than 20,000 patients, when administered subcutaneously initially every two weeks. Trial inclusion criteria include patients with primary hyperlipidaemia or mixed dyslipidaemia who are at risk of clinical cardiovascular events, with and without statin treatment.
B. PCSK9 Genome Editing
Loss-of-function of PCSK9 mutations is found in individuals who have reduced LDL-C levels and reduced cardiovascular disease. In 2014, the identification of loss-of-function mutations that inactivate PCSK9 and lower LDL-C levels were applied to studies in mice. Genome editing with the CRISPR–CRISPR-associated system disrupted the PCSK9 gene in vivo with high efficiency and reduced blood cholesterol levels. This approach may have therapeutic potential for the prevention of cardiovascular disease in humans.
If a PCSK9-specific nuclease system can be designed and delivered to hepatocytes via an adenoviral vector, the possibility of permanent disruption of the PCSK9 gene would mean that a single treatment could be given in the future.
HYPERLIPIDAEMIA TREATMENT GUIDELINES
These recent developments in hyperlipidaemia therapy have seen a re-appraisal of clinical diagnostic and treatment guidelines in Europe and the USA. These can be summarized as follows:
The American College of Cardiology/American Heart Association (ACC/AHA)
For decades, physicians checked LDL or LDL-C levels in their patients and on the basis of these levels, started or adjusted the dose of statins. In 2013, the ACC/AHA developed a ‘risk calculator’ for cardiovascular disease and followed this with their 2014 guidelines. There is a move by ACC/AHA to recommended statin therapy based on patient CAD risk profile, rather than by LDL-C measurement alone.
The National Institute for Health and Care Excellence (NICE) Guidelines
In July 2014, NICE published its guidance (CG181) on cardiovascular risk and lipid modification. In particular, the advice given for starting statin therapy is that this should only be done after an informed discussion between the clinician and the patient about the risks and benefits of treatment. The 2014 NICE guidelines (CG181) also take into account additional factors in deciding to start statin therapy, such as potential benefits from lifestyle modifications, informed patient preference, co-morbidities, other medications and life expectancy. There is a move by NICE to recommended statin therapy based on other clinical risk factors for CAD, rather than by LDL-C measurement alone.
The American Diabetic Association (ADA)
The American Diabetic Association (ADA) 2015 has updated its Standards of Medical Care in Diabetes, published every January as a supplement to Diabetes Care. The ADA has recommended statin therapy by patient ‘ risk profile’ rather than by LDL-C measurement alone. Type II diabetes is a major risk factor for CAD, so the ADA recommends statin use for nearly everyone with diabetes and has provided guidance on starting doses. The ADA acknowledges that there are major evidence gaps concerning lipid lowering and reduction of CAD, such as for patients younger than 40 or older than 75 years and those with type 1 diabetes.
In conclusion, 2015 and 2016 will bring some welcome and interesting developments in the treatment of hyperlipidaemia. With the competition for the next wave of these cardiology blockbuster drugs, some welcome attention can be expected in refining practical treatment guidelines for clinicians and patients.
On January 26th 2015, Regeneron / Sanofi announced that the FDA has accepted its application for alirocumab and has set a deadline of July 24th 2015 for their marketing decision. Amgen’s evolocumab is scheduled to get its FDA ruling by August 27th 2015.
Firstly, a new approach to the removal of ‘bad’ LDL-cholesterol (LDL-C) from the blood includes a novel class of therapeutic monoclonal antibody inhibitors (to the enzyme PCSK9) that show promise in clinical trials.
Second, the safety and efficacy of statin therapy have been re-evaluated, with new recommendations for more widespread use and combination treatment approaches.
Third, 2014 saw the publication of new clinical guidelines on the management of hyperlipidaemia from the National Institute for Health and Care Excellence (NICE), the American College of Cardiology/American Heart Association (ACC/AHA), the European Atherosclerosis Society (EAS), the International Atherosclerosis Society (IAS) and the American Diabetic Association (ADA)..
As for 2015, the race is on for regulatory approval of new potential cardiology ‘blockbuster’ drugs to control hyperlipidaemia. Further into the future comes the possibility of inhibiting the lipid-regulating enzyme, PCSK9, using targeted gene therapy.
THE CASE FOR HYPERLIPIDAEMIA TREATMENT
Cardiovascular disease remains the most common cause of morbidity and mortality worldwide. The underlying disease, atherosclerosis, affects large muscular arteries such as the coronary arteries and also the aorta. Coronary artery atherosclerosis, or coronary artery disease (CAD) causes acute and chronic ischaemic heart disease (IHD), including myocardial infarction (MI) or ‘heart attacks.’
Familial hypercholesterolaemia (FH) is caused mainly by genetic defects in the LDL receptor gene. This genetic defect impairs the ability of the liver to remove LDL-C from the blood. The heterozygous form of the defective gene is inherited from one parent and affects between 1 in 250 and 1 in 300 people worldwide, which makes heterozygous FH one of the most common hereditary condition in humans. The homozygous form of FH is more severe and occurs when a mutated copy of the gene is inherited from both parents and affects between 1 in every 500,000 to 1 in every one million people.
Aside from familial forms of hyperlipidaemia, individuals who are also considered to be at risk of coronary artery disease (CAD) and who are advised to control plasma LDL-C levels include those with diabetes mellitus, hypertension, obesity and smokers.
STATIN THERAPY
For the past two decades, statin therapy, including atorvastatin (Lipitor®) and its generic forms, rosuvastatin (Crestor®) and recently ezetimibe (Zetia®), has been the mainstay of treatment to lower this ‘bad’ cholesterol (LDL-C). In November 2014, the outcome of the IMPROVE-IT clinical trial, an 18,144-patient study of high-risk patients presenting with acute coronary syndromes, showed that patients taking ezetimibe (Zetia®) in combination with simvastatin (Vytorin®) experienced significantly fewer major cardiovascular events.
The dominance of statin therapy in hyperlipidaemia has persisted despite the fact that some patients will be resistant and will maintain high LDL-C levels with treatment while some others will be unable to tolerate statins.
2014 was a year when lowering plasma cholesterol with statins was a key topic in the general media as well as in the medical journals. It was also a year of controversy regarding the safety of statin therapy. In the British Medical Journal (BMJ) meta-analysis data was reported to show that only a small minority of adverse symptoms in patients taking statins were genuinely due to the statins. This media attention came at a time when NICE issued its draft guidance recommending lowering the risk threshold for starting statin treatment. A leading UK epidemiologist stepped in to caution against widespread statin prescribing.
While much of the media attention given in 2014 to hyperlipidaemia treatment was directed at statin therapy, there were some new developments.
PCSK9 INHIBITORS
The enzyme proprotein convertase subtilisin/kexin 9 (PCSK9) is a serum protease, the ninth member of the subtilisin family of kexin-like proconvertases to be identified. PCSK9 sequesters the LDL-cholesterol (LDL-C) receptor in the liver and so reduces plasma levels of LDL-C. In early clinical trials, the reduction in plasma LDL-C that follows PCSK9 inhibition has been shown to be greater (by up to 80%) than with statins alone and PCSK9 have been reported to have fewer side effects. This initial efficacy and safety data explains why the PCSK9 inhibitor class of drugs are predicted to be the next blockbusters in cardiology and why there is a race to develop these inhibitors.
A. PCSK9 Monoclonal Antibody Therapy
PCSK9 inhibitory therapeutic monoclonal antibodies include alirocumab (Sanofi/Regeneron), evolocumab / AMG 145 (Amgen) and bococizumab (Pfizer). These humanized monoclonal antibodies bind to PCSK9. The interest in this therapeutic approach lies in the fact that a single injection may be effective when given weekly, fortnightly or even monthly.
Alirocumab: In October 2013, alirocumab showed promising clinical data in phase 3 clinical trials. The ODYSSEY programme included 12 trials that included more than 23,000 patients with either familial hyperlipidaemia or intolerance to statin therapy. The ODYSSEY MONO trial compared alirocumab with ezetimibe at week 24, with results showing mean LDL-C reductions from baseline of 47.2% on treatment with alirocumab when compared with 15.6% with ezetimibe. In phase 2 trials, alirocumab combined with a statin achieved LDL-C reductions in up to 73% of patients.Preliminary data from the ongoing Odyssey Long Term study, showed that alirocumab halved the number of strokes and heart attacks in heterozygous familial hypercholesterolemia and high-risk cardiovascular patients (1.4 % of alirocumab-treated patients compared with 3% for placebo). Regulatory filings for alirocumab in Europe and the USA are expected during 2015.
Evolocumab (AMG 145): Evolocumab is a humanized therapeutic monoclonal antibody that inhibits PCSK9. Safety and efficacy of evolocumab is being evaluated in a programme of 22 phase 3 clinical trials involving more than 30,000 patients. Evolocumab is administered every two weeks and monthly in multiple patient populations. The name of the programme is PROFICIO (Program to Reduce LDL-C and Cardiovascular Outcomes Following Inhibition of PCSK9 In Different Populations).
Data from the ongoing PROFICIO phase 3 trials, the large MENDEL-2 phase 3 trials in statin-naîve patients and in the GAUSS-2 phase 3 trial in statin-intolerant patients, evolocumab reduced LDL-C levels by more than 50%.Data from the RUTHERFORD-2 clinical trial, published in October 2014, showed that evolocumab was well-tolerated in patients with heterozygous familial hypercholesterolaemia, and gave significant reductions in LDL-C compared with placebo.Data was analyzed at 52 weeks from the DESCARTES long-term safety and efficacy clinical trial in patients with hyperlipidemia at risk for cardiovascular disease. Evolocumab treatment when added to the diet alone, to low-dose atorvastatin (Lipitor®), or to high-dose atorvastatin (Lipitor®) with or without ezetimibe (Zetia®) significantly reduced LDL-C levels.
Following the results of these clinical trials, Amgen has become the first company to seek regulatory approval for a PCSK9 inhibitor. In August 2014, a submission was made of a biologics license application (BLA) to the US Food and Drug Administration (FDA). In September, 2014, a submission of a Marketing Authorization Application (MAA) was made to the European Medicines Agency (EMA). The result of these filings is expected during 2015.
Bococizumab (RN-316): For Pfizer’s therapeutic monoclonal antibody, bococizumab, ongoing large phase 2 and phase 3 clinical trials are due for completion during 2015 and 2016. The safety, efficacy and tolerability of bococizumab is being assessed in more than 20,000 patients, when administered subcutaneously initially every two weeks. Trial inclusion criteria include patients with primary hyperlipidaemia or mixed dyslipidaemia who are at risk of clinical cardiovascular events, with and without statin treatment.
B. PCSK9 Genome Editing
Loss-of-function of PCSK9 mutations is found in individuals who have reduced LDL-C levels and reduced cardiovascular disease. In 2014, the identification of loss-of-function mutations that inactivate PCSK9 and lower LDL-C levels were applied to studies in mice. Genome editing with the CRISPR–CRISPR-associated system disrupted the PCSK9 gene in vivo with high efficiency and reduced blood cholesterol levels. This approach may have therapeutic potential for the prevention of cardiovascular disease in humans.
If a PCSK9-specific nuclease system can be designed and delivered to hepatocytes via an adenoviral vector, the possibility of permanent disruption of the PCSK9 gene would mean that a single treatment could be given in the future.
HYPERLIPIDAEMIA TREATMENT GUIDELINES
These recent developments in hyperlipidaemia therapy have seen a re-appraisal of clinical diagnostic and treatment guidelines in Europe and the USA. These can be summarized as follows:
The American College of Cardiology/American Heart Association (ACC/AHA)
For decades, physicians checked LDL or LDL-C levels in their patients and on the basis of these levels, started or adjusted the dose of statins. In 2013, the ACC/AHA developed a ‘risk calculator’ for cardiovascular disease and followed this with their 2014 guidelines. There is a move by ACC/AHA to recommended statin therapy based on patient CAD risk profile, rather than by LDL-C measurement alone.
The National Institute for Health and Care Excellence (NICE) Guidelines
In July 2014, NICE published its guidance (CG181) on cardiovascular risk and lipid modification. In particular, the advice given for starting statin therapy is that this should only be done after an informed discussion between the clinician and the patient about the risks and benefits of treatment. The 2014 NICE guidelines (CG181) also take into account additional factors in deciding to start statin therapy, such as potential benefits from lifestyle modifications, informed patient preference, co-morbidities, other medications and life expectancy. There is a move by NICE to recommended statin therapy based on other clinical risk factors for CAD, rather than by LDL-C measurement alone.
The American Diabetic Association (ADA)
The American Diabetic Association (ADA) 2015 has updated its Standards of Medical Care in Diabetes, published every January as a supplement to Diabetes Care. The ADA has recommended statin therapy by patient ‘ risk profile’ rather than by LDL-C measurement alone. Type II diabetes is a major risk factor for CAD, so the ADA recommends statin use for nearly everyone with diabetes and has provided guidance on starting doses. The ADA acknowledges that there are major evidence gaps concerning lipid lowering and reduction of CAD, such as for patients younger than 40 or older than 75 years and those with type 1 diabetes.
In conclusion, 2015 and 2016 will bring some welcome and interesting developments in the treatment of hyperlipidaemia. With the competition for the next wave of these cardiology blockbuster drugs, some welcome attention can be expected in refining practical treatment guidelines for clinicians and patients.
On January 26th 2015, Regeneron / Sanofi announced that the FDA has accepted its application for alirocumab and has set a deadline of July 24th 2015 for their marketing decision. Amgen’s evolocumab is scheduled to get its FDA ruling by August 27th 2015.
 RSS Feed
RSS Feed